
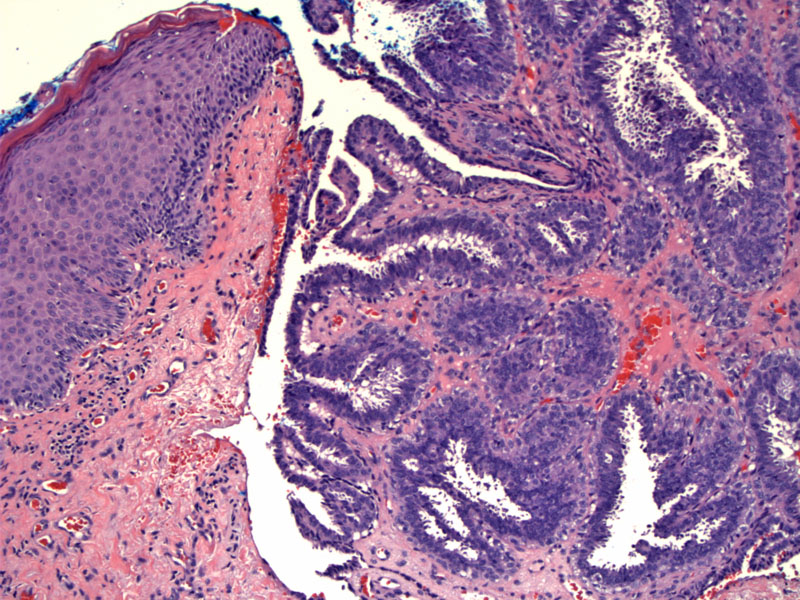
Case 1: A bilayer of epithelium lines papillae. The luminal layer of columnar epithelial cells demonstrate decapitation, where cytoplasmic secretions appear to lift off from the apices. Inside the stroma of the larger papillae, glandular inclusions are seen. Note that the nodule appears to connect with the overlying epithelium, which is not common, but can occur focally.
The spaces formed by the glands and papillae have been described as maze-like. The fronds are lined with a double-layer, but this may be difficult to detect at times.
Hidradenoma papilliferum is a sweat gland neoplasm that presents almost exclusively in the vulva or perianal area of women. Isolated cases of its occurrence in the nipple or eyelid have been reported (McKee).
Microscopically, the well-demarcated nodule is seen in the dermis, consisting of complex papillary structures and "maze-like" glands. The papillae are lined with a double-layer of epithelium, with the outer (basement membrane) layer consisting of myoepithelial cells with hyperchromatic nuclei and a luminal layer of columnar cells with apocrine "decapitation" (bits of cytoplasm appear to bud off from the apices of the columnar cells). Inflammatory cells are sparse.
The nodule is usually not connected to the overlying epidermis, but there may be occasional foci of connectivity. This is in contrast to syringocystadenoma papilliferum, another sweat gland neoplasm with similar histology, but which does connect to the epidermis, is usually located in the head or neck and has prominent plasma cells.
Clinically presents as a solitary nodule (1-2 cm) in the vulva, perineal or perianal regions. The overlying skin may be unaffected or ulcerated.
Excellent. This lesion is benign and vanishingly rare reports of malignancy have been reported in the literature.
• Adnexal : Syringocystadenoma Papilliferum
McKee PH. Pathology of the Skin with Clinical Correlations 2nd Ed. London, UK: Mosby-Wolfe; 1996: pg 15.75-15.76.
Rapini RP.Practical Dermatopathology. Philadelphia, PA: Elsevier; 2005: pg 295.