
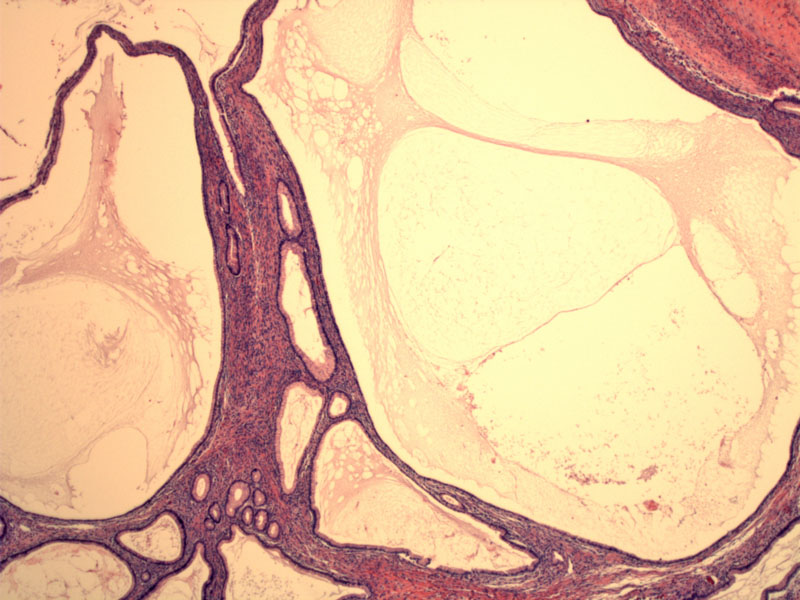
Mucinous cystadenomas consist of simple unilocular or multilocular cysts lined by mucinous epithelium of endocervical or intestinal types. In this example, multiple cysts are lined with an attenuated epithelium. Other smaller cysts are lined by a columnar mucinous epithelium.
Cysts are most commmonly lined with tall columnar cells with clear cytoplasm and bland dark nuclei that are basally oriented.
A higher power demonstrates the bland simple mucinous epithelium. There is no cytologic atypia or pseudostratification.
Occasionally, there may be undulations of the epithelium, forming crypt-like structures or rarely, papillae (not shown here). The lining cells remain simple and bland.
Intestinal-type epithelium with goblet cells is seen in this mucinous cystadenoma. Usually, intentinal-type epithelium is more common in borderline and malignant mucinous tumors, but can occasionally be seen in benign mucinous tumors.
Grossly, the tumor may be firm, rubbery, or soft. The cut surface reveals smooth, thin-walled mucin-filled, multiloculated cysts. The cysts can range from a few millimeters to several centimeters. It is important to check that the lining of the cyst is smooth, as well as the external surface of the ovary. Excrescences and areas of nodularity may suggest areas of borderline or even malignant change.
This particular mucinous cystadenoma had abundant mucin, some of which has extravasated into the stroma. Note that this is not a sign of malignancy in this situation. Pseudomxyoma peritonei, usually due to a mucinous neoplasm of the appendix, may present similarly under the microscopic. However, the dissecting mucin in pseudomyxoma peritonei is more abundant and elicits a stronger stromal reaction. Furthermore, the clinical presentation of pseudomyxoma peritonei will be different.
Mucinous epithelial tumors of the ovary are characterized by epithelial cells that recapitulate endocervical epithelium or gastrointestinal epithelium. They are divided into three categories: (1) mucinous cystadenomas or cystadenofibromas, (2) borderline mucinous tumors (also known as mucinous tumors of low malignant potential), and (3) mucinous carcinomas.
Benign mucinous tumors account for 80% of all mucinous ovarian neoplasms. They are cystic (unilocular or multilocular) masses that are generally unilateral and have a smooth, blue-white or gray external surface with numerous blood vessels. If the stromal component is prominent, they are often termed mucinous cystadenofibromas. Approximately 5% of mucinous cystadenomas are associated with a dermoid cyst or a Brenner tumor.1 They are typically the largest of all ovarian neoplasms. Most are less than 10cm in diameter, but they may reach a diameter of greater than 30 cm!
Microscopically, they are lined by columnar mucinous cells with basally oriented nuclei, resembling endocervical or gastric-type epithelium. Intestinal-type epithelium with goblet cells or Paneth cells are occasionally seen, but this type of epithelium is more common in borderline or malignant mucinous tumors. Ovarian stroma of mucinous cystadenomas is often quite cellular. Foci of stromal luteinization are not infrequent, especially around the periphery of the tumor. Occasionally, the luteinized stromal cells are clinically functional, resulting in estrogenic or androgenic effects.1,2
Rupture of mucinous glands and cysts often occurs during surgical removal, producing small mucin granulomas with numerous macrophages and occasional multinucleated giant cells caused by extravasation of mucinous secretions into the stroma. This must be distinguished from pseudomxyoma peritonei from a mucinous neoplasm of the appendix.1
These tumors occur over a wide age range, but is most common in the reproductive years. The tumors can be quite large, ranging from 1 to over 30 cm in diameter. Though many tumors are incidental findings, larger ones present with abdominal discomfort and fullness.
For example, the patient of this particular case was a 61-year-old G2P2 woman who presented with increasing abdominal distension, pressure, early satiety and a 10 pound weight loss over the past year and a half. She was noted to have a 20 x 30 x 30 cm abdominopelvic mass on CT scan.
Treatment is with cystectomy or oophorectomy.
Excellent; excision is curative.
• Ovary : Mucinous Borderline Tumor, Endocervical-type (Case 2)
• Ovary : Mucinous Cystadenocarcinoma (Infiltrative Type)
1 Hart WR. Mucinous Tumors of the Ovary: A Review. Int J Gynecol Pathol. 2005(24);4-25.
2 Fletcher CDM, ed. Diagnostic Histopathology of Tumors. 3rd Ed. Philadelphia, PA: Elsevier; 2007: 575-6.
2 Nucci MR, Oliva Esther. Gynecologic Pathology: Foundations in Diagnostic Pathology. Philadelphia, PA: Elsevier: 2009: 412-3.