
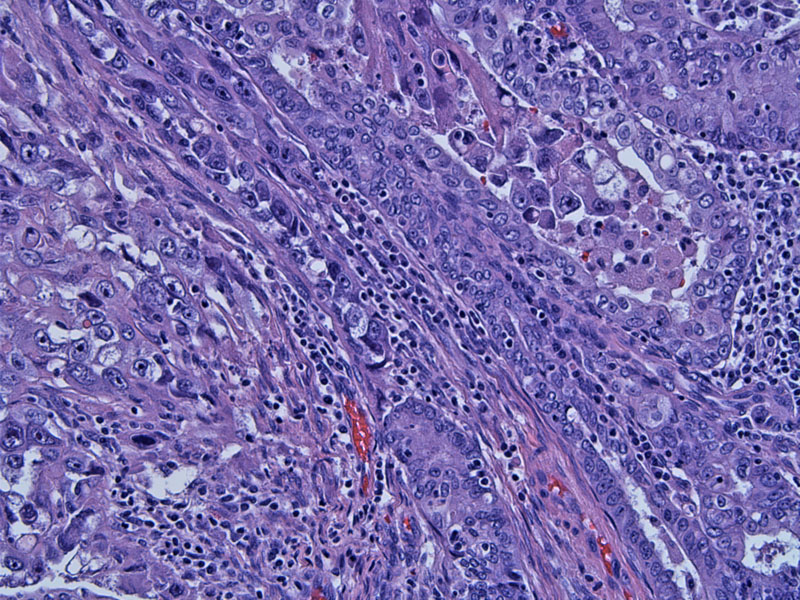
Malignant glands are seen intimately admixed and blending with a high grade undifferentiated sarcomatous component.
The mesenchymal component is comprised of bizarre pleomorphic cells with no specific differentiation.
Another area showing an admixture of the carcinomatous and sarcomatous components. Both can be poorly differentiated and difficult to distinguish from each other. Some authorities surmise that both components may derive from the same stem cell. This 'metaplasic carcinoma' theory is supported by the fact that the sarcomatous component stains positively with epithelial markers.1
Another tumor demonstrates heterologous elements. Bone (seen here) is one of the more frequent elements when heterologous mesenchymal differentiation is present.
Yet another tumor demonstrates immature mesenchymal components and some glandular formation. Although the epithelial components are most often endometrioid or serous endometrial adenocarcinoma, a specific histologic type may not be evident in a poorly-differentiated tumor.
A closer view of the sarcomatous component demonstrates bizarre cells with no particular line of differentiation. Areas of myxoid change (bluish stroma) are seen.
Another area demonstrate an undifferentiated small blue cell component with extensive geographic necrosis.
A different tumor demonstrates a spindle cell sarcomatous component.
Other areas of the tumor shows admixed epithelial components, as seen in this island of pleomorphic poorly-differentiated squamous cells.
Mixed malignant mullerian tumors (carcinosarcomas) are composed of an admixture of malignant epithelial and malignant mesenchymal components. The epithelial component is most frequently a high-grade endometrioid endometrial adenocarcinoma or serous adenocarcinoma. Less commonly, clear cell, mucinous, squamous or undifferentiated carcinomas are seen. The sarcomatous components can be homologous (expressing elements intrinsic to the uterus such as endometrial stroma or leiomyosarcoma) or heterologous (expressing elements extrinsic to the uterus such as rhabodomyosarcoma, benign-appearing cartilege or chondrosarcoma).
In the past, heterologous differentiation was thought to have a more ominous prognosis. It has since been shown that the epithelial component plays a more important role. Serous or clear cell histology connotes a worse prognosis, and it is the epithelial component (not the mesenchymal component) that metastasizes.1
Typically occurs in postmenopausal women; black women are more commonly affected. Presents with abnormal vaginal bleeding and enlarged uterus with the tumor protruding through a dilated cervical os. Risk factors are similar to those of endometrioid endometrial adenocarcinoma and include: unopposed estrogen exposure, obesity, tamoxifen therapay and nulliparity. Use of progestin-containing medications is protective. Approximately a third of women have a history of prior pelvic radiation.1,2
Treatment consists of hysterectomy with bilateral salpingo-oophorectomy, pelvic and peri-aortic lymphadenectomy, and washings for full surgical staging. While no adjuvant therapy has been shown to be successful in preventing recurrences, ifosfamide and platinum based agents are showing some promise in early clinical trials.
Prognosis is poor as these tumors are very aggressive. Stage is the most important prognostic factor. Up to 2/3 of patients present at an advanced stage (Stage III-IV) with the tumor extending outside the uterus. Median survival rate for all stages is approximately 2 years.1,2
• Endometrium : Atypical Polypoid Adenomyoma
• Endometrium : Adenosarcoma with Sarcomatous Overgrowth
1 Fletcher CDM, ed. Diagnostic Histopathology of Tumors. 3rd Ed. Philadelphia, PA: Elsevier; 2007: 663-4.
2 Nucci MR, Oliva Esther. Gynecologic Pathology: Foundations in Diagnostic Pathology. Philadelphia, PA: Elsevier: 2009: 313-7.