
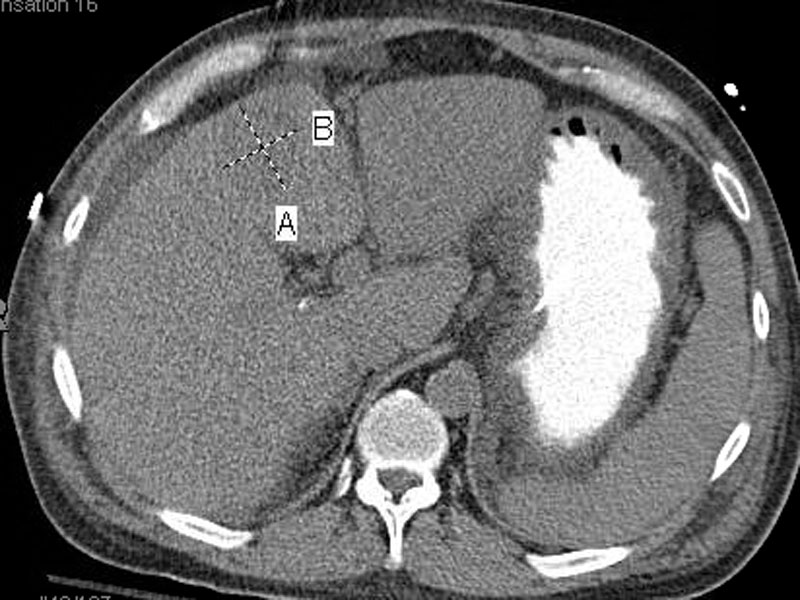
CT of the abdomen shows a 4 cm lesion with ill-defined margins in hepatic segment 4a consistent with a malignant hepatic neoplasm. The liver demonstrates a nodular contour suggestive of cirrhosis.
Imaging from a different patient has more extensive liver involvement by hepatocellular carcinoma. This CT scan shows a nodular liver with a heterogeneous infiltrating mass involving most of the right lobe. Small satellite lesions were also present in the left lobe. The dashed line indicates a tumor thrombus involving the main portal vein extending to the superior mesenteric vein.
HCC have three classic growth patterns: trabecular (recapitulating normal liver cell plates), solid and tubular (which may mimic bile duct carcinoma). This core biopsy demonstrates a well-differentiated HCC with a trabecular pattern and thickened cell plates.
The resection of the above core biopsy showed similar trabecular growth of the tumor.
Gross image of above tumor: HCC may be unifocal, multifocal or diffusely infiltrative. In this image, the lesion is well-circumscribed, against a background of cirrhosis. The tumor is paler than the surrounding liver parenchyma and may be green (not shown here) if the well-differentiated hepatocytes are capable of secreting bile.
This poorly differentiated tumor displays prominent nuclear pleomorphism.
Another area of this tumor, demonstrating significant nuclear pleomorphism with prominent nucleoli, tumor giant cells, and a lack of any architectural pattern (trabecular or tubular).
Another area illustrates numerous mitoses, another feature of poorly differentiated HCC.
Because HCC have a strong propensity to invade vascular channels, intrahepatic metastasis often occurs with this manner. Here is a gross image of another case demonstrating intrahepatic spread of HCC.
Gross image of another lesion, which is a more poorly-differentiated tumor microscopically (see image below). This tumor is larger, less well-circumscribed with intrahepatic spread, as demonstrated by a smaller separate nodule to the right of the main lesion.
Diff quick shows a cellular lesion without evident trabecular architecture.
The cells are polyhedral and have centrally placed nuclei compatible with hepatocellular differentiation. However, the architecture is highly disturbed.
The pap stained smear shows overlapping nuclei and cells growing in sheets rather than thin trabecular units.
The corresponding cell block confirms cells which are clearly hepatocellular in differentiation, but show high nuclear to cytoplasmic ratios and disorganized growth.
Hep par immunostaining shows diffuse cytoplasmic positivity, further corroborating the hepatocellular nature of the lesion.
The rare fibrolamellar variant of hepatocellular carcinoma shows round cells with deeply eosinophilic cytoplasmic surrounded by a dense fibroblastic backround. Unlike conventional hepatocellular carcinoma, the adjacent liver typically lacks cirrhosis and hepatitis.
Again the hypercellularity of the hepatocellular lesion is evident, with lack of a trabecular growth.
Hepatocellular carcinoma is one of the most common cancers in the world, especially Asia and Africa. There are some general differences in epidemiology and etiology between HCC cases in high-incidence countries (e.g. Southeast China, Mozambique) to lower incidence countries in Western Europe and North America.
~85% of HCC cases occur in countries with high incidence of chronic HBV infection. Infection generally occurs in infancy via vertical transmission from infected mothers, and this confers a 200-fold increased risk of HCC by adulthood. Cirrhosis may be present or absent and HCC develops at age 20-40. Note that the development cirrhosis is an important, but not requisite, factor in the development of HCC. In contrast, in the Western world, cirrhosis is usually present (85-95%) of cases, usually in the setting of chronic liver disease from alcohol, HCV and hereditary hemochromatosis. HCC develops at a later age, generally after 60.1
Predisposing conditions for HCC include the following:
- Viral infection (HBV and HCV): For example, integration of HBV into the DNA of hepatocytes is found to precedes malignant transformation.
- Chronic alcoholism: repeated cycles of cell death and regeneration as seen in chronic hepatic injury may predipose to HCC due to accumulations of mutations during cell division.
- Environmental toxins: Aspergillus flavus found in moldy grains and peanuts are carcinogenic. Specially, they bind to DNA and cause mutations in proto-oncogenes and tumor suppressor genes.
- Tyrosinemia: 40% of patients with this metabolic disease develop HCC despite following dietary restrctions.
- Hereditary hemochromatosis: in the cirrhotic stage, up to 27% develop HCC.
More common in men; occurs after age 50, but may be earlier in endemic countries. Presents with abdominal pain, ascites and liver enlargement. Progression of disease leads to liver failure and metastasis (favorite site is lung). Extension of tumor may occlude portal vein or inferior vena cava, even growing into the right side of the heart!1
Elevations of serum AFP (alpha-fetoprotein) occurs in a significant percentage of HCC cases. AFP elevation can also occur in malignant germ cell tumors (ie. yolk sac tumors), cirrhosis, hepatitis, liver necrosis, normal pregnancy and fetal neural tube defects. However, if AFP levels are 100 times normal and maligant germ cell tumor can be excluded, then, it is virtually diagnostic of HCC.2
Individuals with HCC are often poor surgical candidates because of reduced hepatic function as a result of coexisting cirrhosis or the presence of multiple tumors. The treatment options for patients with cirrhosis and HCC depends on many factors, such as patient age, tumor stage, liver function, and donor availability.A meta-analysis showed that in patients with small HCC, treatment with radiofrequency ablation is superior to treatment with percutaneous ethanol injection. Small HCCs were defined according to the Milano criteria as solitary HCC <5 cm or with up to 3 nodules smaller than 3 cm
For those with larger tumors, liver transplantation appears ideally
suited, as it involves complete oncologic resection and correction of the
underlying liver dysfunction. Large tumor size is a significant factor of poor survival after hepatic resection in patients with HCC, although several investigators have also reported that this factor was not significant.
Universal HBV vaccination of children in endemic areas may decrease incidence of HCC.1
Extremely poor if untreated, with 5 year survival rate of 3% in the US. With resection, the 5 year survival rates can range from 25-65%.2 . For those few who do undergo transplantation, evidence supports that vascular invasion is a major determinant of the outcome. HCC can recur even in the allograft as well as in distant sites after complete tumor removal, suggesting that circulating malignancy cells might be responsible for recurrences. Overall, the topic is complicated but in a nutshell, survival for HCC patients with cirrhosis who undergo hepatic resection can be stratified on the basis of alkaline phosphatase value, tumor size, satellite lesions, and vascular invasion.
1 Kumar V, Abbas AK, Fausto N. Robbins and Cotran Pathologic Basis of Disease. 7th Ed. Philadelphia, PA: Elsevier; 2005: 924-6.
2 Rosai, J. Rosai and Ackerman's Surgical Pathology. 9th Ed. Philadelphia, PA: Elsevier; 2004:994-1003.
Ambrogio Orlando et al. Radiofrequency Thermal Ablation vs. Percutaneous Ethanol Injection for Small Hepatocellular Carcinoma in Cirrhosis: Meta-Analysis of Randomized Controlled TrialsAm J Gastroenterol 2009 br /br /
Mazzaferro V, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med 1996;334:693–9.
Yeh CN, Chen MF, Lee WC, Jeng LB.J Prognostic factors of hepatic resection for hepatocellular carcinoma with cirrhosis: univariate and multivariate analysis.Surg Oncol. 2002 Dec;81(4):195-202.