
Author: Garth Olson MD, Associate Professor, Division of Otolaryngology, University of New Mexico School of Medicine
Co-author(s): Cecelia Wu MD, Department of Pathology, University of New Mexico School of Medicine
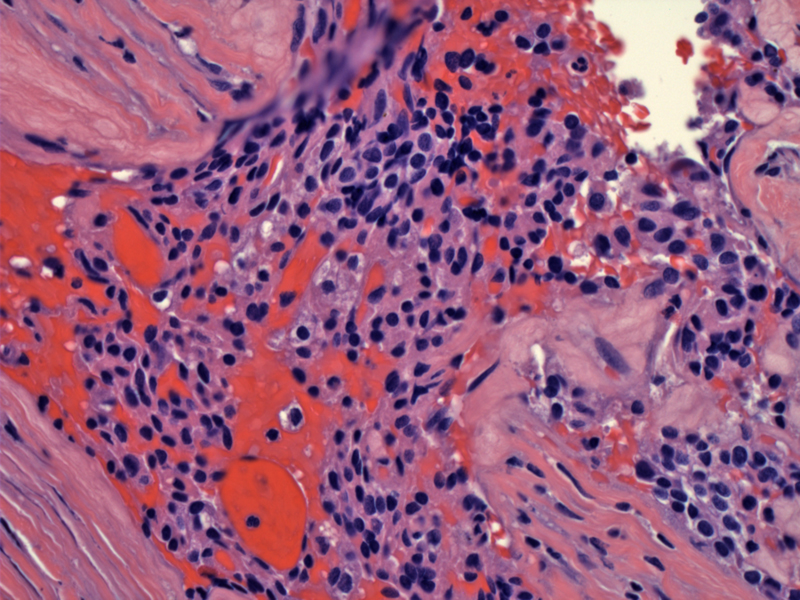
Fairly monotonous neoplastic chief cells are gaining access to a vascular structure. The diagnosis for a parathyroid carcinoma can be made if either of the following criteria are met: (1) tumor invasion into surrounding issues or (2) documented metastasis. However, if invasion or metastasis cannot be identified, then one must rely on a constellation of softer signs such as vascular invasion.
Expanded tumor nodules within a background of broad fibrous septae is another feature suggestive of malignancy. Note that the identification of broad fibrous bands is not sufficient, it must be accompanied by the expansile nodules of neoplastic cells (Fletcher).
Vascular invasion (a tumor embolus in seen inside the vessel in the center) is an extremely helpul feature of malignancy, but is seen in less than 25% of cases.
This different case also shows bands of fibrosis in a proliferative background. However, closer inspection reveals hemosiderin and a well-demarcated capsule. This patient has previously had resection of parathyroid tissue, which resulted in features simulating carcinoma in the remaining hyperplastic glands.
Parathyroid carcinoma is a rare cause of primary hyperparathyroisism (HPT), accounting from 0.5-5% of cases of primary HPT. One frequently cited article estimates the percentage as about 2.1% (Obara). The genetic basis of parathyroid carcinoma has been established with a mutation of the HRPT2 gene on chromosome 1, also expressed in sporadic cases of the disease. HRPT2 is a tumor suppressor gene which codes for parafibromin, a protein with an as yet unknown role. It's thought that this gene is involved in regulation of the cell cycle and proliferation.
Germline mutations of the HRPT2 gene are also responsible for familial hyperparathyroidism, and the rare hyperparathyroidism-jaw tumor syndrome. Hyperparathyroidism-jaw tumor syndrome consists of parathyroid adenoma (or carcinoma), fibro-osseous tumors of the jaw and kidney tumors (Carpten).
Because cellular pleomorphism can be seen in parathyroid adenomas, it is not a helpful feature in distinguishing between adenomas and carcinomas. Two features (if present) definitively diagnose parathyroid carcinoma and they are (1) invasion into local structures such as the thyroid, esophagus or soft tissue and (2) documented metastasis.
Other softer signs include capsular invasion, vascular invasion, increased mitotic activity (>5 per 10 HPF), broad fibrous bands dividing the parenchyma, coagulative necrosis, monotonous sheets of tumor cells with high N/C ratio, macronucleoli (Fletcher). One must be careful when evaluating for capsular invasion. Previous surgical manipulation may cause scarring and distortion of benign parathyroid tissue, thus mimicking capsular invasion or the presence of the broad fibrous septae that divides expansile nodules ... features seen in parathyroid carcinoma.
UpToDate has done a nice job summarizing the clinical presentation teased from four major papers on the subject with 314 patients total (Fuleihan). We won't rehash the whole article here but it is worth reading. The highlights of the presentations in this patient population are:
- Age: 44 to 54 years
- Mean serum calcium: 14.6-15.9 mg/dL
- Patients with serum calcium concentration > 14 mg/dL: 65-75%
- Neck mass: 34-52%
- Bone disease: 34-73%
- Renal disease: 32-70%
- Pancreatitis: 0-15 %
- Asymptomatic presentation: 2-7%
Again, see the referenced web article for more in-depth analysis3 . It's also interesting that the male to female ratio is 1:1 in parathyroid carcinoma versus the accepted figure of 3:1 for parathyroid adenomas. The main take-home message from all these figures is that patients with parathyroid carcinoma are more likely to present with severe symptoms and lab values for calcium and parathyroid hormone way way above normal. The classic resident pimp question is about a patient with HPT and a neck mass - think parathyroid carcinoma.
Having a high index of suspicion preoperatively should prompt close examination of frozen sections for the mentioned diagnostic signs of parathyroid carcinoma and a more aggressive surgical approach.
Surgical treatment involves excision of the offending gland and adjacent tissue. Typically this involves a partial thyroidectomy, and paratracheal dissection. Because adjuvant therapy is pretty disappointing, clear margins are especially important, and may necessitate nerve sacrifice or other extended procedures such as thymectomy and airway resection and reconstruction. In cases of distant metastasis, resection of lung metastsis has been advocated to reduce the symptoms of hypercalcemia.
At this stage, patients are also typically managed with bisphosphonates and calcimimetics to reduce calcium levels. Chemotherapy and radiation therapy are both more or less investigational in this rare disease and generally have not showed great promise, although there are case report showing some limited responses (Chow). The bottom line is that an aggressive and complete resection up front gives patients the best chance for long-term survival.
Hypercalcemia the main source of morbidity and mortality from parathyroid carcinoma (Obara). The carcinomas grow very slowly in most patients, but can occasionally be aggressive. Approximately one third of patients are cured at initially with surgery, one third have late recurrent disease which can be successfully addressed with further surgical resection, and one third of patients exhibit especially aggressive disease course and succumb to their disease early despite treatment (Hoelting).
• Parathyroid : Hyperplasia simulating Carcinoma
Carpten, JD, Robbins, CM, Villablanca, A, Forsberg, L. HRPT2, encoding parafibromin, is mutated in hyperparathyroidism-jaw tumor syndrome. Nat Genet 2002; 32:676.
Chow, E, Tsang, RW, Brierley, JD, et al. Parathyroid carcinoma — the Princess Margaret Hospital experience. Int J Radiat Oncol Biol Phys 1998; 41:569.
Fletcher CDM, ed. Diagnostic Histopathology of Tumors. 3rd Ed. Philadelphia, PA: Elsevier; 2007: 1087-1091.
Fuleihan GE, Arnold A. Parathyroid carcinoma: UpToDate. UpToDate article on Parathyroid Carcinoma
Hoelting, T, Weber, T, Werner, J, Herfarth, C. Surgical treatment of parathyroid carcinoma (Review). Oncol Rep 2001; 8:931.
Obara, T, Fujimoto, Y. Diagnosis and treatment of patients with parathyroid carcinoma: An update and review. World J Surg 1991; 15:738.