System: Hematopathology: Bone Marrow: Neoplastic: Multiple Myeloma

System: Hematopathology: Bone Marrow: Neoplastic: Multiple Myeloma


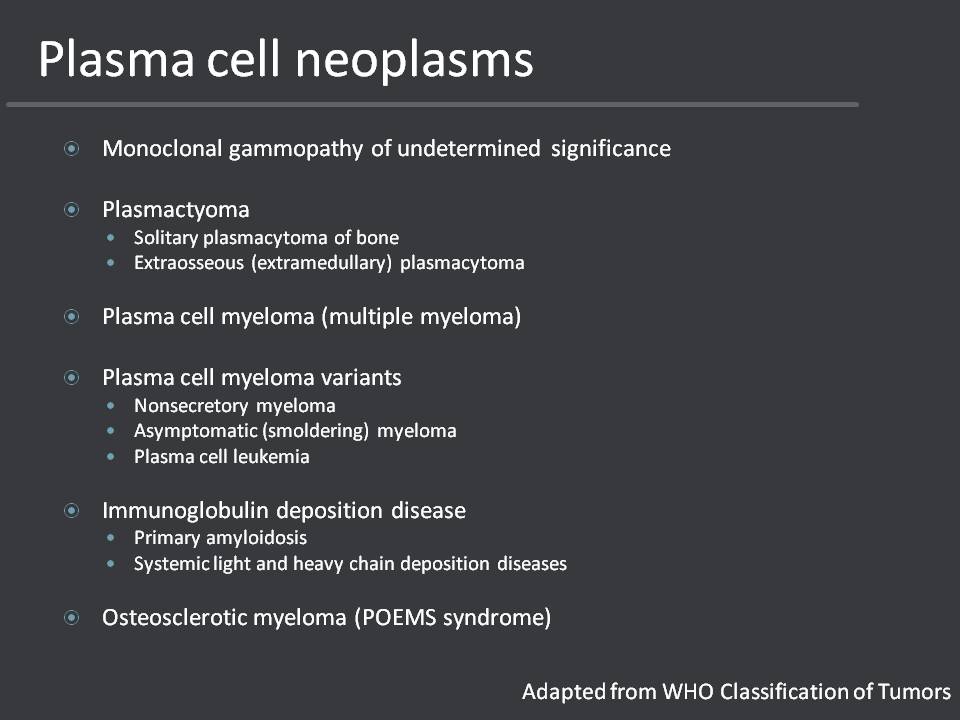
Plasma cell neoplasms consist of a variety of entities with the most common being multiple myeloma
The diagnostic criteria for the diagnosis of multiple myeloma are based off clinical, radiographic, and pathologic findings.
MRI imaging shows an enhancing soft tissue mass entirely replaces a 7 cm segment of the medullary space of the distal femoral diametaphysis and erupts through large segments of the femoral cortex. Reactive edema is present in the medial tibial plateaus, associated with cartilage loss.
Sheets of plasma cells replaced the normal osseous architecture.
Multinucleation (arrow) and pleomorphism and rare findings in a reactive plasma process and should favor the diagnosis of a neoplastic process.
Perinuclear hofs and dense clumped nuclear chromatin in a
The presence of mitotic activity along with atypical nuclei and nucleolation favor a neoplastic process.
Multiple myeloma is a clonal plasma cell neoplasm centered in the bone marrow that is associated with systemic findings and the production of monoclonal immunoglobulins (M-protein). It is the most common form of the plasma cell neoplasms mentioned in the slide above. The majority of individuals affected are older than 50 with the peak incidence around 70. Men are more frequently affected than women and there is a two-fold increase in African Americans. The diagnosis of multiple myeloma is based on the combination of clinical, radiographic, and pathologic findings.
Clinically, patients have an elevated M-protein in the serum or urine. While there is no defined cutoff, patients usually have a serum IgG level >30 g/L, a serum IgA level >25 g/L, or a urine light chain production of 1 g/24hrs. Other clinical findings include hypercalcemia secondary to osteolytic lesions, renal dysfunction due to acute tubular necrosis from Ig light chains, and anemia from bone marrow infiltration and renal dysfunction.
Radiographically, patients have lytic lesions involving the axial skeleton.
Pathologically, there is a clonal plasma cell infiltrate on bone marrow biopsy that generally exceeds 10%. Bone marrow involvement may be patchy and the distribution pattern can range from focal to interstitial to diffuse, or a combination of these. The plasma cells may vary from very immature blastic forms to fully mature plasma cells.
In addition to classic multiple myeloma, there are three clinical variants: asymptomatic (smoldering) plasma cell myeloma, non-secretory myeloma, and plasma cell leukemia. Asymptomatic myeloma is characterized by the presence of an elevated M-protein in the serum and/or >10% involvement of the bone by a clonal plasma cell population in the absence of systemic organ involvement seen in the classic form. Patients with non-secretory myeloma have all the findings of myeloma without M-proteins in the serum or urine. The plasma cell leukemia variant is characterized by the presence of a plasma cell proliferation in the peripheral blood.
If patients present to their doctor with complaints, it is usually related to the multi focal involvement of myeloma. They may present with a pathologic fracture or bone pain, fatigue or infection. Patients are often diagnosed as the result of abnormal laboratory findings related to the underlying process. They may have anemia, hypercalcemia, proteinuria, elevated creatinine or other signs of kidney failure.
The mainstay of therapy used to be oral chemotherapy. Now, there is a drive to incorporate autologous stem cell transplantation into the treatment if eligible.
The median survival is 3-4 years for patients with symptomatic myeloma. There are two different staging systems for multiple myeloma: the Durie-Salmon staging system and the International Staging System (ISS). The Durie-Salmon system stages individuals based on the M-protein level, extent of lytic bone lesions, and the blood and serum hemoglobin, calcium and creatinine levels. The ISS looks at the serum beta2-microglobulin and serum albumin levels. In addition to the clinical staging, abnormal cytogenetic finding (especially deletion of chromosome 13 or hypodiploidy) have negative prognostic implications. Other findings that decrease the median survival include t(4;14), t(14;16), t(14;20), and deletion of 17p on FISH.
Mills SE, ed. Sternberg's Diagnostic Surgical Pathology. 5th ed. Philadelphia, PA: Lippincoott Williams & Wilkins; 2009: 657-60.
Rosai, J. Rosai and Ackerman’s Surgical Pathology, 10th Ed. Philadelphia, PA: Elsevier; 2011: 1980-3.
Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, Thiele J, Vardiman JW (Eds). WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. Lyon: IRAC Press; 2008: 200-8.
The International Myeloma Working Group. Criteria for the classification of monoclonal gammopathies, multiple myeloma and related disorders: a report of the International Myeloma Working Group. British Journal of Haematology. 2003;121:749–57.