System: Skin: Adnexal: Sweat Gland Neoplasm: Hidradenocarcinoma

System: Skin: Adnexal: Sweat Gland Neoplasm: Hidradenocarcinoma


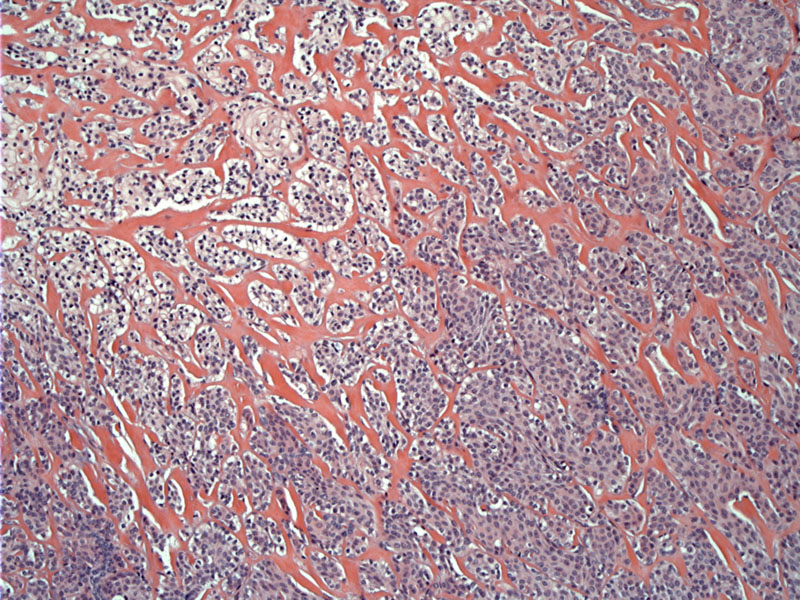
Case 1: Medium power shows a proliferation of epithelioid cells arranged in solid nests of varying size. Some glycogenation of the cells is noted, imparting a clear cell appearance. The nests are infiltrative into the surrounding densely collagenized stroma.
This photomicrograph shows the tumor cells adjacent to a normal eccrine duct (lower right).
A collagenized stroma envelops the cells. One study noted stromal retraction around tumor cells as a histologic feature of malignancy Kazakov
Mucin production is not often noted in hidradenocarcinoma but has been reported in the literature.Nash
Tumor cells are epithelioid with cytoplasmic clearing and prominent nucleoli. Tubule/gland formation is not prominent. Mitotic figures are scarce in this example.
Hidradenocarcinomas usually arise de novo, but can occasionally arise from a pre-existing hidradenoma. Similar to its benign counterpart, hidradenomcarcinomas often exhibit a nodular growth pattern and clear cell change.
This rare malignant sweat gland tumor may be only mildly atypical or frankly malignant. The neoplastic cells have eosinophilic to pale glycogen-containing cytoplasm and distinct cell membranes. Ductal structures will be scattered within the solid nests of tumor cells, which is helpful in distinguishing this entity from squamous cell carcinoma or trichilemmal carcinoma, which lack ductal structures (Busam).
Features of malignancy include infiltrative pattern of growth, increased mitotic activity and a desmoplastic stromal reaction (Kazakov). If one is lucky, the tumor will arise adjacent to a preexisting apocrine hidradenoma, offering a benign example for comparison.
This tumor occurs in all age groups, though it occurs more frequently in older individuals. The face and extremities are favored locations and the tumor presents as a 1-5 cm ulcerated, erythematous nodule.
Treatment involves wide surgical excision with negative margins of at least 2 cm. Selective lymph node biopsy is a common practice. Her-2 amplifications by immunohistochemistry have been reported and one case showed improvement with Herceptin (Nash), but a larger study failed to show Her-2 amplification by FISH in the 14 cases studied (Kazakov).
Local recurrence is common, even with the wide margins noted above. Incomplete resection may result in recurrence or metastasis. The jury still seems to be out on the topic of using Herceptin for these tumors (Kazakov).
Busam KJ. Dermatopathology: Foundations in Diagnostic Pathology 1st Ed. Philadelphia, PA: Elsevier; 2010: 420-1.
Kazakov DV. et al. Cutaneous Hidradenocarcinoma: A Clinicopathological,Immunohistochemical, and Molecular Biologic Study of 14 Cases, Including Her2/neu Gene Expression/Amplification, TP53 Gene Mutation Analysis, and t(11;19) Translocation. Am J Dermatopathol. 2009;31(3):236-247.
Nash JW, Barrett TL, Kies M, et al. Metastatic hidradenocarcinoma with demonstration of Her-2/neu gene amplification by fluorescence in situhybridization: potential treatment implications. J Cutan Pathol. 2007;34:49–54.
Silverberg SG. Silverberg's Principles and Practice of Surgical Pathology and Cytopathology. Philadelphia, PA: Elsevier; 2006:PAGE 262..
Wahl CE, Todd DH, Binder SW, Cassarino DS. Apocrine hidradenocarcinoma showing Paget’s disease and mucinous metaplasia. J Cutan Pathol. 2009; 36: 582–585.
Weedon D, Strutton G, Rubin AI. Skin Pathology. 3rd Ed. London, England, UK: Elsevier; 2010 Page 804.