System: Gastrointestinal: Pancreas: Neoplastic: Solid Pseudopapillary Neoplasm

System: Gastrointestinal: Pancreas: Neoplastic: Solid Pseudopapillary Neoplasm


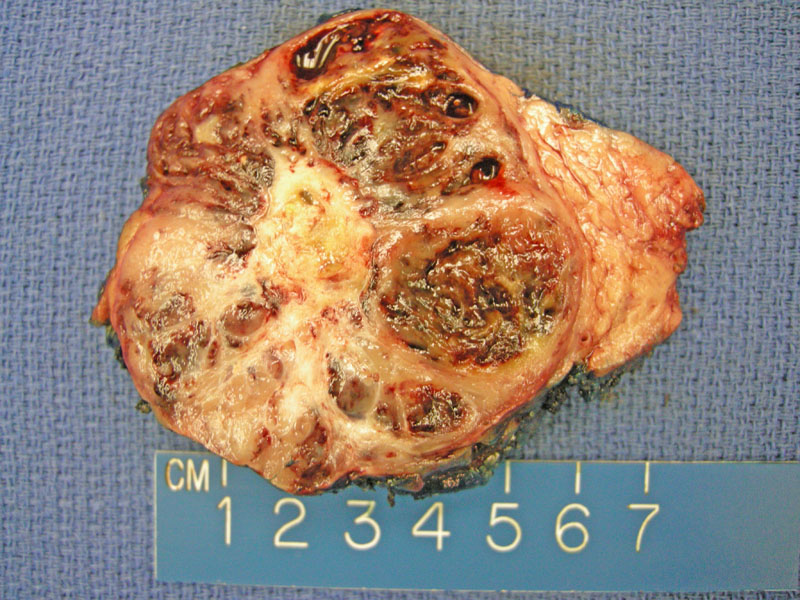
The typical gross appearance shows solid tan areas with admixed hemorrhagic nodules. While degenerative changes such as this are common, actual tumor necrosis is not expected. Oddly enough, there is striking similarity between this particular tumor and a serous microcystic adenoma with the formation of cysts and a central stellate scar, but microscopically, these tumors are quite different.
Solid pseudopapillary neoplasm consists of uniform polygonal cells with delicate capillaries.
The stroma can be minimal, or become markedly hyalinized or myxoid.
Blood lakes along the periphery are not uncommon, with associated hemosiderin laden macrophages.
Areas of pseudopapillary structures may be surrounded by such blood lakes. Degenerative changes result in loss of cohesion, leaving the capillary-sized vessels surrounded by a cuff of neoplastic cells, hence leading to the characteristic pseudopapillary appearance
Areas of clear cells or even cytoplasmic vacuolization are often encountered.
Hyalinization of stroma is focal, surrounded by sheets of neoplastic cells.
Some tumors contain distinct eosinophilic hyaline globules as seen in this image.
Vimentin is uniformly positive in this neoplasm.
Neuron specific enolase is typically strongly positive.
If a neuroendocrine tumor is considered, a negative keratin stain is helpful for corroborating solid pseudopapillary neoplasm. Although not illustrated here, recent studies have shown that most of these tumors demonstrate nuclear β-catenin and loss of membrane expression of E-cadherin (Kim). CD10 has also been shown to be positive in many cases.
FNA often shows a papillary structure. Neoplastic cells with finely granular chromatin and inconspicuous nucleoli surround a vascular core.
classic case from mich Image
higher power Image
Solid-pseudopapillary tumors are uncommon indolent neoplasm generally occurring in young women in their 20s. These tumors may arise anywhere in the pancreas; there is no predilection for any specific location.
Grossly, they are well-demarcated and encapsulated, with variable solid and cystic areas. Often, they contain hemorrhagic and necrotic foci. Microscopically, there are nests and sheets of uniform appearing cells with eosinophilic cytoplasm. The cells can have a cleared-out appearance. Foamy macrophages may be present, as well as hyaline globules and cholesterol crystals. The loss and degeneration of cells furthest from delicate vessels form the pseudopapillae (Weidner).
They often cause few symptoms and may reach a large size by the time they are detected. If symptomatic, the most common symptoms are abdominal pain and a palpable, nontender, upper abdominal mass. By CT and MRI, the tumor is often well circumscribed, encapsulated, and heterogeneous with hemorrhagic and cystic degeneration (Chakhachiro).
Different surgical excisions are employed depending on tumor location. Distal pancreatectomy and central pancreatectomy for tumors of the tail and body, whereas pancreaticoduodenectomy is required for tumors of the pancreatic head. Even locally invasive tumors and limited metastasis can be managed surgically (Panieri).
Good prognosis-- when confined to the pancreas, up to 95% of patients are cured following surgical excision. Even patients with non-resectable or metastatic tumors may show prolonged survival.
→Arises in young women.
→Histologically characterized by pseudopapillae formed by loss of cells away from vessels. Foamy macrophages, eosinophilic globules and cholesterol clefts may be present.
→Most have mutations in beta-catenin gene, leading to abnormal nuclear and cytoplasmic staning.
Chakhachiro ZI, Zaatari G. Solid-pseudopapillary neoplasm: a pancreatic enigma.
Arch Pathol Lab Med. 2009 Dec;133(12):1989-93.
Kim MJ et al. Loss of E-cadherin and cytoplasmic-nuclear expression of β-catenin are the most useful immunoprofiles in the diagnosis of solid-pseudopapillary neoplasm of the pancreas. Hum Pathol 2008. 39:251–258
Nakagohri T, et al. Surgical outcome of solid pseudopapillary tumor of the pancreas. J Hepatobiliary Pancreat Surg. 2008;15(3):318-21.
Panieri E et al. Operative management of papillary cystic neoplasms of the pancreas. J Am Coll Surg 1998. 186:319–324.
Weidner N, et al. Modern Surgical Pathology Philadelphia, PA: Saunders 2003: 896-7.