
This case demonstrates CIN II or moderate dyplasia with immature atypical cells involving the lower 2/3 of the epithelium. There is maturation (albeit abnormal maturation) at the superficial layers. Note the disordered syncytial growth of cells with indistinct cell borders and crowding at the parabasal layers.
Partial extension into an endocervical gland is demonstrated here. Glandular involvement is uncommon in CIN I, but quite common in CIN II or CIN III.
More extensive involvement of an endocervical gland is seen in this image. The outline of the normal gland is largely retained. Extension of dysplastic epithelium into a gland may be mistaken for invasion, however, the smooth rounded border and lack of desmoplasia are diagnostic clues for glandular involvement rather than true invasion.
Another example of a fairly straight-forward moderate dysplasia is seen here with some glandular extension
A different case of CIN II/CIN III is seen here. Atypia extends throughout all layers of the epithelium with only the slightest hint of maturation toward the superficial layers. Koilocytic change is appreciated at the top layers (small perinuclear halos and raisinoid nuclei). Note the mitotic figure in the mid portion of the epithelium. In CIN II, mitoses is largely confined to the lower two-thirds of the epithelium, whereas in CIN III, mitoses can occur at all levels. A thin layer of abnormal parakeratosis is seen at the superfical surface -- also a common finding in severe dysplasia.
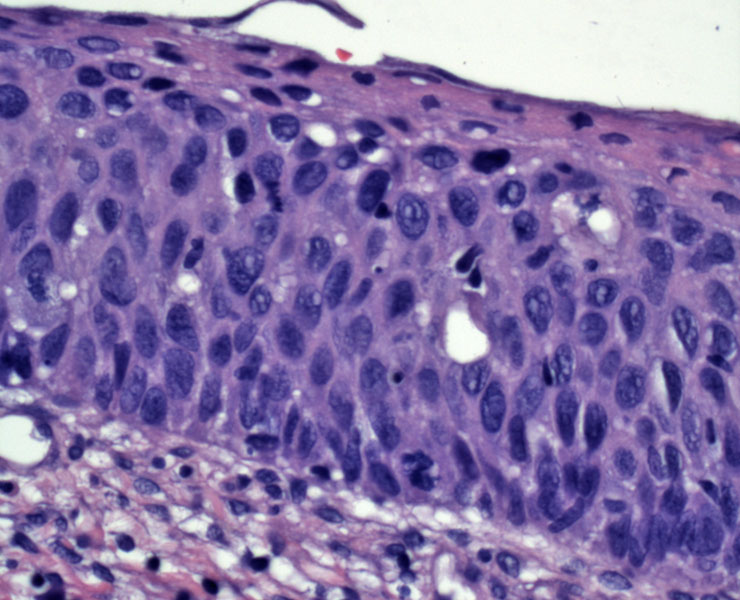
This image clearly demonstrates all the features of severe dyplasia or CIN III. There is no maturation whatsoever at the superficial layer. The nuclei are immature, hyperchromatic and pleomorphic. There is disarray at all levels and a mitotic figure is seen at the top right.
The diagnosis can be a bit more problematic when the epithelium is limited to only a few cells thick and the cells are not elongated and crowded. In this case, the epithelium in infiltrated by neutrophils and there is marked spongiosis and no cellular overlap -- but the nuclei are hyperchromatic.
Moderate dysplasia is seen in the Pap smear as small sheets of cells with immature appearing cytoplasm and hyperchromasia. The cells appear parabasal almost, with cyanophilic cytoplasm. The nuclei are enlarged but occupy less than 50% of the cell.
Hyperchromatic small cells could easily be missed but should be recognized as HGSIL. There is scant cytoplasm, with the nuclei occupying greater than 50% of the cell, consistent with severe dysplasia of non-keratinizing type.
Again, the HGSIL cells show darker, more immature cytoplasm and marked nuclear abnormalities including folds. Nucleoli are not present.
High grade cells from a conventional Pap smear show elongation and scant cytoplasm with coarse hyperchromatic nuclei indicative of a high grade lesion.
Note that when high grade dysplasia colonizes endocervical glands, elongation arises and may simulate AGUS (atypical glandular cells of unknown significance). Sometimes it is even difficult to exclude the possibility of a co-existing glandular lesion.
Three-dimensional cell clusters of small cells which are difficult to see through are a feature which should be inspected closely for the possibility of dysplasia. This patient had extensive severe dysplasia, with many single dysplastic cells along with these 3-D clusters.
In high grade dysplasia, the Ki-67 stain shows nuclear reactivity in all layers of the epithelium including the superficial portion.
In this strip of squamous epithelium (with maturation towards the upper right), there is diffuse strong p16 staining consistent with a high grade lesion.
Again, in this case -- the p16 (left) and Ki-67 (right) immunohistochemistry is particular useful to substantiate the diagnosis of HGSIL.
Sometimes in endocervical curettage specimens, small single squamous cells with dysplastic nuclei are evasive.
In this situation, p16 immunostaining helps illuminate the greater number of dysplastic cells than initially appreciated. This patient's corresponding cervical biopsy confirmed moderate dysplasia.
In LGSIL or CIN I, cytologic atypia is seen only the superficial layers and the basal layers are unaffected. When atypia appears in the basal layers of epithelium, the lesion has progressed to CIN II (moderate dysplasia) or CIN III (severe dysplasia). Note that HGSIL encompasses both CIN II and CIN III.
In CIN II, the lower two-thirds of the epithelium are immature atypical cells, however, there is maturation at the superficial layers, although the maturation is abnormal and produces an odd-looking prickle and keratinizing cell layer.1 Furthermore, mitotic figures are confined to the lower two-thirds of the epithelium.
CIN III occurs when immature atypical cells involve all layers of the epithelium. Mitotic figures are seen at all levels.
High grade dysplasia reflects viral activity at the basal layers of the epithelium. As viral gene products E6 and E7 degrade host tumor suppressor p53 and hypophosphorylated RB, the cell cycle is disrupted and uncontrolled proliferation occurs. As a compensatory response, p16INK4 (a cell cycle inhibitor) is upregulated and often can be detected by IHC. Thus, strong staining of p16INK4 supports the diagnosis of a high-grade lesion. Note that high-grade lesions are usually the result of infection by a high-risk HPV subtype (ie. HPV 16 or 18). Ki-67, a marker of proliferative activity, will also stain strongly in high-grade lesions.1,2
HGSIL is often asymptomatic and is detected on cervical cytologic screening. On colposcopy using dilute acetic acid, regions of the cervix with HGSIL are often characterized as densely acetowhite, with straight margins, and punctate or large branching vessels.
As HGSIL has a high risk of malignant progression, treatment is performed via cervical cone biopsy. This both eliminates the lesion as well as diagnoses any coincident lesions missed on colposcopic biopsy. As cervical cone biopsies are associated with preterm deliveries in subsequent pregnancies, younger women with robust immune systems are often given the option of expectant management with close surveillance.
HGSIL has a high risk of malignant progression, which often occurs over several years. Immunocompromised patients are at risk for a more rapid disease progression.
→HGSIL encompasses CIN II and CIN III.
→CIN II exhibits some maturation at the upper third of the epithelium whereas CIN III displays full-thickness atypia.
→Mitotic figures in CIN II is limited to the lower 2/3 of the epithelium whereas CIN III can have mitotic figures throughout all levels of the epithelium.
→In a Pap smear, the hyperchromatic atypical nuclei occupy less than 50% of the cell in CIN I and more than 50% of the cell in CIN III.
→IHC stains for p16 and Ki-67 can help you identify HGSIL.
→Interestingly, p16 (a cell cycle inhibitor) is upregulated as a compensatory mechanism, and thus, is often employed as a proxy marker for HPV infection.
• Cervix : Low grade squamous intraepithelial lesion
1 Kumar V, Abbas AK, Fausto N. Robbins and Cotran Pathologic Basis of Disease. 7th Ed. Philadelphia, PA: Elsevier; 2005: 1073-77.
2 Nucci MR, Oliva Esther. Gynecologic Pathology: Foundations in Diagnostic Pathology. Philadelphia, PA: Elsevier: 2009: 147-156.