
This was para-aortic paraganglioma weighing 21 grams. Note the festooning and somewhat nested pattern of growth. The classic
Clusters of neoplastic cells with salt and pepper chromatin form around some hyalinized cores.
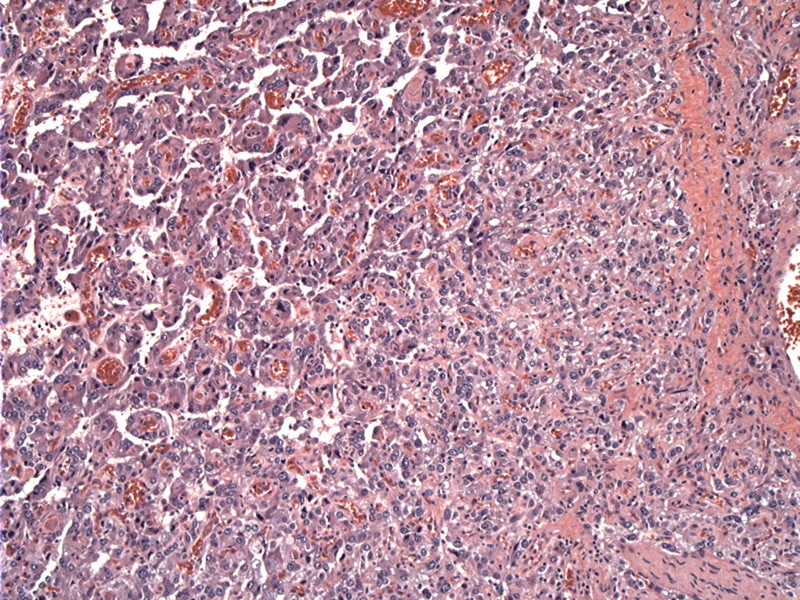
Larger areas of hemorrhage (blood lakes) are seen in other ares of the tumor.
Size and shape variation of the neoplastic cells can be present. Atypia and pleomorphism are not reliable indicators of malignancy. A tumor capsule is seen at bottom.
In terms of IHC, the chief cells are reactive for NSE, synaptophysin and chromogranin. This image shows diffusely positive chromogranin in the neoplastic chief cells. The most specific and reliable neuroendocrine marker currently used in pathology practice remains chromogranin A.
The neoplastic cells are also positive for NSE.
S100 highlights the sustentacular cells.
Paragangliomas are the extra-adrenal counterpart of pheochromocytomas. Paraganglia can exist in several locations: (1) head and neck (2) along either side of the spine and abdominal aorta and(3) rare sites such as bladder, heart and thyroid.
The paravertebral paraganglia extends from the neck to the pelvis, and along with the adrenal medulla, forms the sympathoadrenal neuroendocrine system. In the newborn, the organ of Zuckerkandl is a large aggregate of paraganglia on either side of the aorta (usually at the bifurcation or origin), sometimes joined in the midline by an isthmus (Fletcher). This organ regresses to some residual tissue (identical to the adrenal medulla) in adulthood, but of course, paragangliomas can arise in this tissue and from any paraganglia.
Note that the paraganglia in the head and neck is more closely aligned with the parasympathetic nervous system, whereas the paravertebral/paraaortic paraganglia function closely with the sympathetic nervous system. Thus, the prototypic sympathetic ganglia are the adrenal medulla and organ of Zuckerkandl and prototypic parasympathetic ganglion is the carotid body (Tischler).
Histologically, paravertebral and paraaortic paragangliomas have identical histology to that seen in the head and neck. Clusters of chief cells in a "Zellballen" pattern are separated by stroma and vasculature. A trabecular pattern with broad interconnecting cords can also be common. The neoplastic cells have the usual salt and pepper chromatin pattern and occasionally intracytoplasmic hyaline globules (Fletcher).
In medical school, one was taught the rule of 10s. 10% familial, 10% malignant, 10% extra-adrenal, 10% bilateral and 10% pediatric. However, recent studies have found that approximately 30% of these tumors arise in a familial (inherited) setting. This number may even increase as we accrue knowledge about germline mutations and molecular mechanisms of oncogenesis.
The hereditary syndromes (thus far) shown to be associated with pheochromocytomas include: MEN2A, MEN2B (RET mutation on 10q11), von Hippel-Lindau (VHL on 3p25-26), neurofibromatosis type I (NF1 on 17q11) and familial paraganglioma due to mutations of succinate dehydrogenase genes SDHD, SDHC, SDHB. These SDH genes also appear to have a tumor suppressor function (Tischler).
Location of an extra-adrenal paraganglioma has some influence on biologic behavior-- carotid body paragangliomas, for example, have a relatively low rate of malignant behavior, while extra-adrenal retroperitoneal paragangliomas tend to have a higher incidence of clinically malignant behavior.
Aorticopulmonary paragangliomas may be functionally active, while those in the head and neck are not.
Carney Triad describes the coexistence of several tumors, including gastric epithelioid GIST, pulmonary chondroma, and extra-adrenal paraganglioma.
• Neck : Paraganglioma (Carotid Body)
Fletcher CDM, ed. Diagnostic Histopathology of Tumors. 3rd Ed. Philadelphia, PA: Elsevier; 2007: 1769-70.
Tischler AS. Pheochromocytoma and extra-adrenal paraganglioma: updates. Arch Pathol Lab Med. 2008 Aug;132(8):1272-84.
