
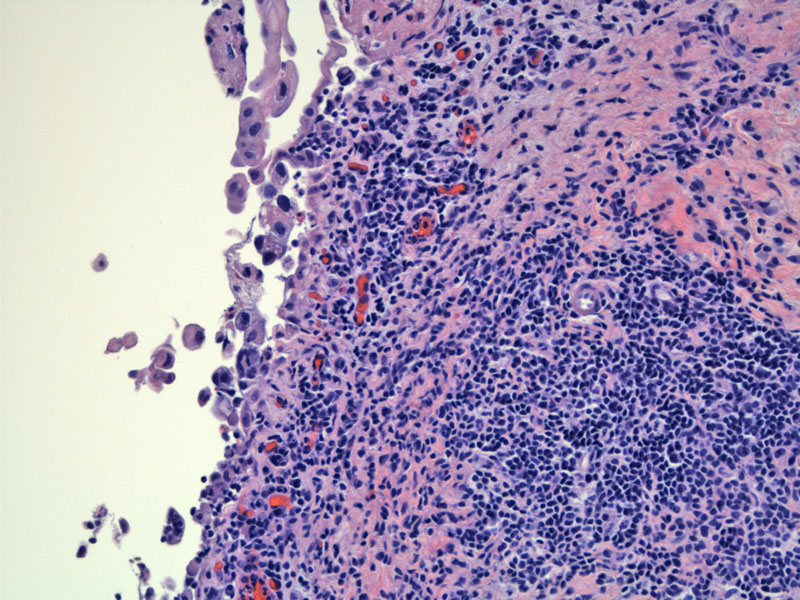
This biopsy shows inflamed mucosa with denuding cells. Close inspection of the nuclear features show hyperchromasia and enlargment, consistent with carcinoma in situ.
For those not fully convinced, an adjacent area on the same biopsy shows small aggregates of denuded epithelial cells.
Higher power of this area shows nulear enlargment and irregular outlines, along with hyperchromasia.
The corresponding urine sample on this case shows degenerative changes and a few intact single cells with hyperchromatic nuclei. Cohesive groups are lacking.
The lower half demonstrates confluent CIS while the right upper half of the image shows normal urothelium. Loss of polarity, increased N/C ratio and prominent nucleoli can be seen.
Large cells with dark nuclei are concentrated in the left portion of the image, with a few CIS cells admixed with normal appearing epithelium to the right.
Full thickness CIS (left) is seen here with irregular enlarged hyperchromatic urothelial cells transition to normal (right).
CIS commonly shows loss of cellular cohesion, with areas of individual cell sloughing.
Despite the cytoplasmic degeneration due to the denuded nature of these cells, the malignant nature is still evident in the urine cytology specimen.
This area of CIS shows pink cytoplasmic globules, interestingly.
2004 WHO/ISUP Classification of Urothelial Neoplasms
Urothelial (transitional cell) neoplasms represent ~90% of all bladder tumors, and the remainder consist of squamous cell carcinoma, adenocarcinoma, small cell carcinoma and sarcomas.1 Although mainly located in the bladder, these lesions can occur anywhere where there is urothelium such as the renal pelvis and urethra. Transitional cell carcinomas are divided into two main categories: papillary and flat (sessile) types.
- Papillary lesions encompass benign papillomas, papillary urothelial neoplasm of low malignant potential (PUNLUMP), papillary urothelial carcinoma low and high grade. These lesions are thought to arise from papillary urothelial hyperplasia. A point of clarification: Even though the term carcinoma is used in the later two entities, these lesions are NOT invasive. When the tumor cells invade the lamina propria and muscularis propria, the additional term invasive urothelial cell carcinoma carcinoma is used. Yes, very confusing.
- Flat lesions also have a spectrum, ranging from mild atypia and displasia to carcinoma in situ (CIS).
Therefore, transitional cell carcinomas have two precursor lesions: noninvasive papillary carcinomas and CIS.
CIS is synonymous with high-grade dysplasia, therefore, malignant cells with similar characteristics as high-grade papillary carcinoma must be present to make this diagnosis. Unlike papillary types, an increase in the layer of cells is not important. Even if a single layer of malignant cells is present, a diagnosis of CIS can be made. Again, the key is the presence of high-grade malignant cells.
CIS can have a pagetoid pattern of growth, where the malignant cells percolate along the basement membrane.
Grossly, the bladder mucosa may be erythematous, granular and edematous. CIS is often multifocal. Because of the unique tendency of CIS to be discohesive, they slough off and will often be found in urine cytology specimens.
CIS is often found in association with high-grade and invasive papillary carcinomas, although some CIS lesions appeared to be isolated. If untreated, 50-67% of CIS will eventually progress to invasive transitional cell carcinoma.1,3
• Bladder : Transitional Cell Carcinoma, High Grade (Invasive)
• Bladder : Radiation Cystitis
1 Kumar V, Abbas AK, Fausto N. Robbins and Cotran Pathologic Basis of Disease. 7th Ed. Philadelphia, PA: Elsevier; 2005: 1028-1033.
2 Fletcher CDM, ed. Diagnostic Histopathology of Tumors. 3rd Ed. Philadelphia, PA: Elsevier; 2007: 526-537.
3 Rosai, J. Rosai and Ackerman's Surgical Pathology. 9th Ed. Philadelphia, PA: Elsevier; 2004:1333-4.