
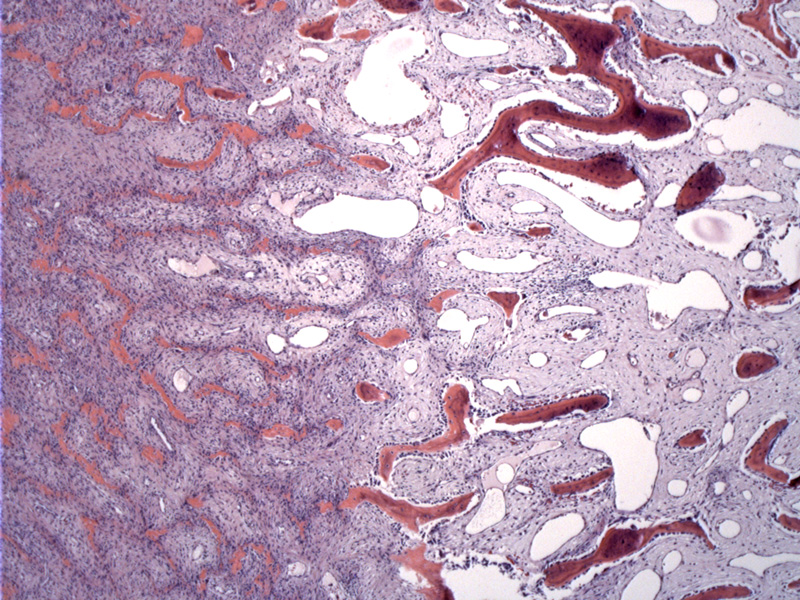
At low power, the pathognomonic zonation can be appreciated. Spindled myofibroblasts evolve into osteoid, immature woven bone and finally to mature trabecular bone.
A proliferation of spindled cells in a loosely textured myxoid stroma. The transition is more abrupt in some areas.
Osteoblastic rimming is seen in the woven bone.
The scattered bony trabeculae surrounded by spindle cells are reminiscent of fibrous dysplasia in some areas. However, fibrous dysplasia is a reactive lesion within the actual bone whereas myositis ossificans occurs in the soft tissue, but forms metaplastic bone.
Myositis ossificans (heterotopic ossification) is a reactive lesion that develops in skeletal muscle after trauma. It is a soft tissue tumor that elaborates bone and cartilege.
The appearance of the lesion will vary depending on the time since injury. On imaging, early lesions appear as a non-specific tissue mass whereas later lesions appear as ossified nodules. Grossly, MO is usually less than 5 cm. Early lesions are solid, grey with a gritty surface representing calcifications. More developed lesions are often completely ossified, required a bonesaw to bisect.
Histologically, early lesions are very cellular and spindled (may resemble a sarcoma) whereas later lesions have developed mature lamellar bone. There is a cellular proliferation of spindled or plump myofibroblastic cells with vesicular nuclei. The background stroma is variably myxoid or collagenous. Mitotic figures are common (never atypical forms) and necrosis is absent.
Osteoid emanates from the myofibroblastic cells, which gradually transitions to more mineralized woven bone with osteoblastic rimming and eventually becoming mature lamellar bone. This gradual evolution of spindle cells to osteoid to immature woven bone to lamellar bone is called the "zoning phenomenon" and is fairly unique to myositis ossificans.
Fibro-osseous pseudotumor of the digits is virtually indistinguishable from myositis ossificans, however, it arises in the nonmuscular soft tissues of the digits. Early myositis ossificans can mimic nodular fasciitis, however, nodular fasciitis occurs in the superficial soft tissues and rarely contains bone. Soft tissue osteosarcoma, an important entity to exclude, arises in older patients and exhibits hemorrhage, necrosis and plemorphism (Folpe).
Ossifying fibromyxoid tumor is similar to myositis ossificans in that there is a proliferating of plump or spindled cells with a peripheral shell of mature bone. However, OFT occurs in older adults, present as a subcutaneous nodule (hence more superficial location), is more lobulated separated by fibrous septae, and the cells are more rounded rather than spindled.
Usually occurs in young adults with equal gender predilection. Patients present with rapid enlargement, pain and swelling in large muscle groups of the proximal extremities or trunk. Sometimes, patients do not recall a history of trauma.
Radiographs show a lesion with an egg-shell rim of bone. It is not attached to bone, unlike osteosarcoma.
Excision may be required if the lesion is large, painful, or causes issues with mobility. Sometimes excision is necessary to make the diagnosis.
Benign; simple excision is curative. Recurrence is uncommon.
→Occurs in young adults, often with a history of trauma.
→A characteristic "zoning phenomenon" is seen histologically with the gradual transition of spindled cells, which merge into osteoid that becomes immature woven bone and mature trabeculae bone.
• Fibrous : Fibro-osseous Pseudotumor of Digits
• Uncertain Lineage : Ossifying Fibromyxoid Tumor
• Fibro-osseous : Fibrous Dysplasia
• Osseous : Conventional Osteosarcoma, High Grade
Fletcher CDM, ed. Diagnostic Histopathology of Tumors. 3rd Ed. Philadelphia, PA: Elsevier; 2007: 1639-40.
Folpe AL, Inwards CY. Bone and Soft Tissue Pathology: Foundations in Diagnostic Pathology Philadelphia, PA: Elsevier; 2010: 239-241.
