System: Skin: Adnexal: Sebaceous Neoplasm: Sebaceoma

System: Skin: Adnexal: Sebaceous Neoplasm: Sebaceoma


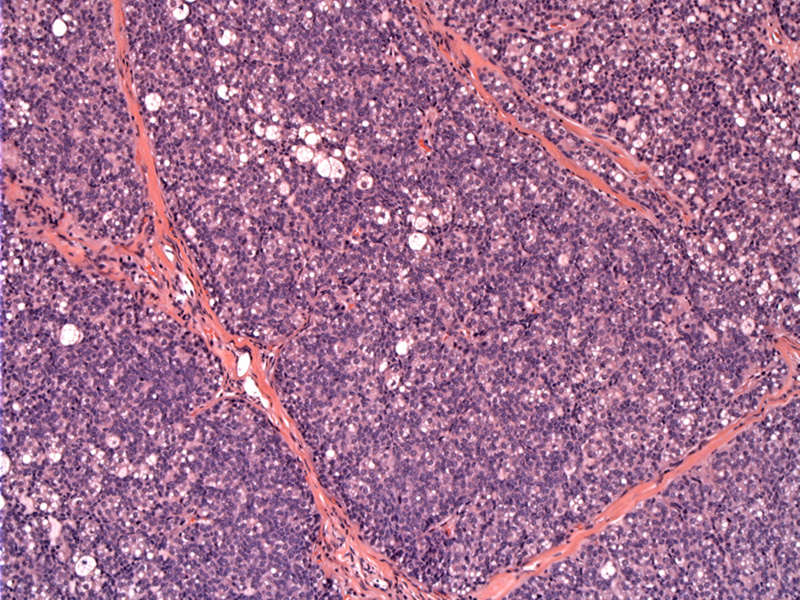
Case 1: Sebaceoma is largely comprised of nodules of basaloid cells, with a random admixture of mature vacuolated sebocytes. The lobules are surrounded by a fibrotic stroma.
The small, uniform basaloid cells and sebocytes demonstrate mild atypia in the form of nucleoli. Pleomorphism and necrosis are not identified. Scattered (minimal) mitoses may be present. Cysts and duct-like structures my be found (see bottom left corner).
Sebaceomas can occur sporadically, as a part of the Muir-Torre syndrome (see clinical description below) or in association with nevus sebaceous. Sebaceomas represent a benign neoplasm with a behavior and histologic appearance somewhat inbetween sebaceous adenoma and sebaceous carcinoma. While they can be locally infiltrative, they do not have metastatic potential like sebaceous carcinoma. Sebaceous adenomas contain a majority of mature sebocytes arranged in lobules, as opposed to a majority of basaloid germinative cells seen in sebaceoma.
Due to the predominance of basaolid cells, basal cell carcinoma with sebaceous differentiation is part of the differential. However, sebaceomas do not demonstrate the palisading and clefting characteristic of basal cell carcinoma. Sebaceomas exhibit monomorphic basaloid cells arranged in a benign appearing architectural pattern with absent/minimal mitotic activity, whereas BCC with sebaceous differentiation have pleomorphic basaloid cells in a malignant architectural pattern with brisk mitotic activity (Alsaad). IHC can also help in this distinction, as sebaceous neoplasms are positive for CK7 while basal cell carcinomas are not (Weedon).
Sebaceomas usually occur as solitary flesh colored nodules on the face or scalp of adults. If multiple tumors are present, Muir-Torre Syndrome may be considered. Muir-Torre Syndrome is an autosomal dominant variant of Lynch syndrome (defect in DNA mismatch repair) characterized by multiple tumors of sebaceous differentiation in addition to visceral malignancy, usually of the GI or GU tract.
The most commonly mutated mismatch repair genes in Muir Torre Syndrome is MSH2 and MLH1, though all of the most common mismatch repair genes (MLH1, MSH2, MSH6 and PMS2) are screened for by immunohistochemistry, just as in GI tumors suspected of arising from this syndrome. Those with Muir-Torre syndrome tend to develop visceral malignancy before sebaceous tumors, nevertheless, MSI in sebaceous tumors can be used as a way to screen for this syndrome in the case of a negative colonoscopy (Weedon).
Treatment of solitary lesions includes excision, primarily for cosmetic reasons (Eisen). Should one suspect a defect in mismatch repair, screening with immunohistochemistry for mismatch repair genes may be indicated.
→Like all tumors of sebaceous glands, sebaceoma (if multiple) may be associated with Muir-Torre syndrome.
→Sebaceoma is considered a histologic variant of sebaceous adenoma, but with an abundance of basaloid epithelial cells.
→The key differential diagnosis for a sebaceoma is BCC with sebaceous differentiation.
• Adnexal : Sebaceous Carcinoma
Alsaad KO, et al. Skin adnexal neoplasms - part 1: An approach to tumors of the pilosebaceous unit. J Clin Pathol 2007;60:129-44.
Eisen DB, Michael DJ. Sebaceous lesions and their associated syndromes: part I. J Am Acad Dermatol. 2009;61(4):549-60.
Weedon D, Strutton G, Rubin AI. Skin Pathology. 3rd Ed. London, England, UK: Elsevier; 2010 Page 776.