
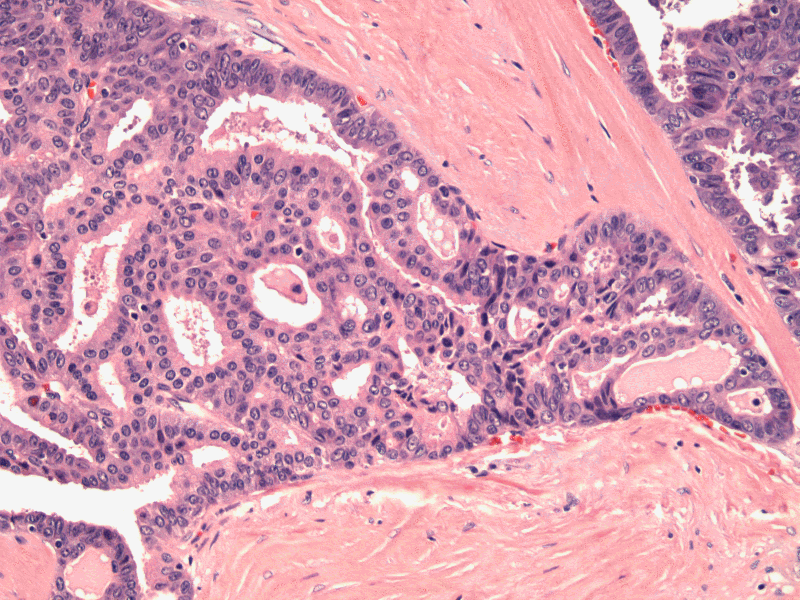
Other areas of the same tumor shows less classic morphology. TCV usually forms trabeculae or papillae, but here are forming variably sized follicles.
On low power, the tall cell variant fills the slide field, with little intervening uninvolved background areas.
In addition to the 2:1 height to width criteria, other features of tall cell variant include oncocytic cytoplasm and nuclear features characteristic of papillary thyroid carcinoma such as nuclear clearing, irregularities and grooves and pseudoinclusions.
Here is a more solid region. The height to width ratio is not 2:1 in some areas. But the nuclear features are typical of PTC (crowding, grooves, clearing, prominent nucleoli) and other areas of the tumor are more classic for tall cell.
Oncocytic cytoplasm is due to abundant mitochondria.
Case 2: Cytology shows round to oval nuclei with abundant cytoplasm.
Corresponding surgical resection to this smear shows extensive tall cells with widespread soft tissue and nodal involvement.
Cell borders are discernible with crowded, ground-glass nuclei. The cytoplasm is eosinophilic.
Papillary thyroid carcinoma (PTC), for the most part, is relatively indolent. However, there are several variants which have a more aggressive course, the most common of which is the tall cell variant (TCV). TCV is more likely to exhibit extra thyroidal extension, distant metastasis, and resistance to radioactive iodine therapy compared to conventional PTC.
Depending on which paper or textbook you read, the percentage of tall cells comprising the tumor necessary for the diagnosis of TCV ranges from 30-70%, and the height to width ratio of the individual tall cells can be 2:1 or 3:1. However, it is important to establish clear criteria since the diagnosis of TCV has significant prognostic implications and the entity is often underdiagnosed.
Ghossein and Livoisi (2008) propose the following criteria for TCV:
- Tumor composed of greater or equal to 50% tall cells
- Tall cell height should be at least twice its width
- Eosinophilic cytoplasm in tall cells
- Nuclear features characteristic of papillary thyroid carcinoma
Fletcher notes that the current WHO classification has tightened the diagnostic criteria and TCV should be composed predominantly of tumor cells with a height width ratio of at least 3:1. Most other experts currently still stick to a ratio of 2:1. However, as Fletcher notes, it may not be a disservice to the patient if the tall cell morphology is not missed as the tumor will exhibit other more obvious signs of this aggressive variant (e.g. large size, extrathyroidal extension).
TCV should distinguished from the columnar cell variant, which is characterized by even taller cells, pseudostratified elongated nuclei and hyperchromatic nuclei (Fletcher).
Molecular studies have identified an overexpression of Muc1 and point mutations in the proto-oncogene B-RAF. Muc1 is an epithelial transmembrane protein whose overexpression can interfere with cell adhesion, thus promoting the discohesiveness and exodus of malignant cells. B-RAF mutations are identified in 80% of TCV, and are a hallmark of aggressive behavior in thyroid cancers. For example, conventional PTC with B-RAF mutations demonstrate higher rates of nodal metastasis than B-RAF negative tumors (Ghossein).
The most common genetic alteration in papillary thyroid carcinomas is the RET/PTC rearrangement. Interestingly, this rearrangment shows geographic variation and occurs in approximately 35% of PTC in North America. There are over 10 different variation of RET/PTC rearrangements, but the RET/PTC1 and RET/PTC3 account for over 90% of cases. There is evidence that the RET/PTC1 rearrangement is seen more in typical PTC with an indolent clinical course, whereas the RET/PTC3 rearrangement occurs more frequently in more aggressive variants such as the tall cell and solid variants (Nikiforov, Basolo).
TCV presents in older patients and is more likely to exhibit extra thyroidal extension than conventional PTC. One study quoted 80% of extra thyroidal extension in TCV (vs 3% in PTC), and the age of presentation in TCV was 53 (vs 45 in PTC) (Ostrowski).
The B-RAF mutation common to TCV may become a target of therapy (anti-B-RAF therapy), which would be most welcome development as a significant proportion of TCV is refractory to radioactive iodine therapy. Furthermore, many of them present with extra thyroid extension and metastases.
In a study conducted by Leung et al (2008), the 10 year survival rate of TCV is 48% compared to 93% of conventional PTC.
→Tall cell variant is composed predominately of tumor cells with a height:width ratio of 2:1 or 3:1.
→This variant is usually bulkier and more likely to show extrathyroidal extension.
→B-RAF mutation is common
• Thyroid : Papillary Thyroid Carcinoma, Cribriform-Morular Type
• Thyroid : Papillary Carcinoma, Oncocytic Variant
• Thyroid : Papillary Thyroid Carcinoma
• Thyroid : Papillary Carcinoma, Solid Variant
• Thyroid : Papillary Carcinoma, Columnar Variant
• Thyroid : Papillary Carcinoma, Follicular Variant
• Thyroid : Papillary Carcinoma, Warthin's Variant
• Thyroid : Papillary Carcinoma, Columnar Variant
Basolo F, Giannini R, Monaco C, et al. Potent mitogenicity of the RET/PTC3 oncogene correlates with its prevalence in tall-cell variant of papillary thyroid carcinoma. Am J Pathol. 2002 Jan;160(1):247-54.
Fletcher CDM, ed. Diagnostic Histopathology of Tumors. 3rd Ed. Philadelphia, PA: Elsevier; 2007: 1008-1009.
Ghossein R, Livoisi VA. Papillary Thyroid Carcinoma Tall Cell Variant. Thyroid(2008)18:1179-1181.
Leung AK, Chow SM, Law SC. Clinical features and outcome of the tall cell variant of papillary thyroid carcinoma. Laryngoscope. 2008 Jan;118(1):32-8.
Nikiforov YE. RET/PTC rearrangement in thyroid tumors. Endocr Pathol. 2002 Spring;13(1):3-16.
Ostrowski MI, Merino MJ. Tall cell variant of papillary thyroid carcinoma: a reassessment and immunohistochemical study with comparison to the usual type of papillary carcinoma of the thyroid. Am J Surg Pathol (1996) 20:964-974.